The Impact Areas Questionnaire (IAQ): A Music Therapy Service Evaluation Tool
DOI:
https://doi.org/10.15845/voices.v20i2.2816Parole chiave:
service evaluation, impact areas, tool, Impact Areas Questionnaire (IAQ), Nordoff RobbinsAbstract
L’Impact Areas Questionnaire (IAQ): uno strumento di valutazione del servizio di musicoterapia
La valutazione del servizio è un requisito professionale per gli esperti e le organizzazioni di musicoterapia. Tuttavia, i risultati della valutazione del servizio sono raramente pubblicati nella letteratura professionale, e la documentazione su processi e metodi di tali valutazioni è limitata, inclusi la logica, i dilemmi e le sfide incontrate. Probabilmente, ciò è dovuto allo stato percepito, alle carenze metodologiche e alla specificità del contesto del lavoro di valutazione del servizio. Attingendo al nostro impegno con la valutazione del servizio in diversi contesti, siamo diventati consapevoli del suo potenziale oltre i suoi tipici usi attuali sul campo, nonché della necessità di una discussione e un dibattito aperto sugli strumenti di valutazione disponibili. È qui che si trova l'obiettivo di questo articolo: introdurre uno strumento di valutazione del servizio, Impact Areas Questionnaire (IAQ), insieme agli studi che hanno portato alla sua costruzione. Sviluppato originariamente attraverso una revisione di 27 progetti, il questionario contiene una serie di diverse aree di impatto. Adottando una prospettiva ecologica, queste aree fanno riferimento all'impatto percepito della musicoterapia non solo sugli utenti dei servizi, ma anche su famiglie, caregivers, amici, personale e contesto organizzativo nella sua interezza. A seguito del suo sviluppo originale all'interno dei centri Nordoff Robbins in Inghilterra e Galles, il questionario è stato testato nel contesto Nordoff Robbins in Scozia con l'obiettivo di esplorarne l'applicabilità e la trasferibilità ad altri contesti di musicoterapia. Oltre a presentare i risultati del test, si discute il potenziale uso dell'IAQ, il quale è incluso come appendice a questo articolo, in altri contesti, e della sua rilevanza per la conoscenza e l'elaborazione di politiche sul campo.
Traduzione di Claudio Cominardi
Riferimenti bibliografici
Abrams, B. (2010). Evidence-based music therapy practice: An integral understanding. Journal of Music Therapy, 47(4), 351-379, https://doi.org/10.1093/jmt/47.4.351.
Ansdell, G. (2006). Response to Tia DeNora. British Journal of Music Therapy, 20(2), 96-99.
Baines, S. (2014). Giving voice to service user choice: Music therapy as an anti-oppressive practice (Doctoral dissertation). University of Limerick, Ireland.
Bennett, R. (2017). Acts of service: The role of a two-fold moral purpose in Nordoff-Robbins music therapy. In G. Tsiris, G. Ansdell, N. Spiro, & O. Coggins (Eds.), Exploring the spiritual in music: Interdisciplinary dialogues in music, wellbeing and education (p. 24). Nordoff Robbins.
Bieleninik, Ł., Geretsegger, M., Mössler, K., Assmus, J., Thompson, G., Gattino, G., Elefant, C., Gottfried, T., Igliozzi, R., Muratori, F., Suvini, F., Kim, J., Crawford, M., Odell-Miller, H., Oldfield, A., Casey, Ó., Finnemann, J., Carpente, J., Park, Al., Grossi, E., & Gold, C. (2017). Effects of improvisational music therapy vs enhanced standard care on symptom severity among children with autism spectrum disorder: The TIME-A randomized clinical trial. Journal of the American Medical Association, 318(6), 525-535, https://doi.org/10.1001/jama.2017.9478.
Bradt, J. (2018). Involving services users in music therapy evaluation. Nordic Journal of Music Therapy, 27(1), 1-2, https://doi.org/10.1080/08098131.2018.1398973.
Bradt, L., & Dileo, C. (2010). Music therapy for end-of-life care. Cochrane Database of Systematic Reviews, 2010(1), CD007169, https://doi.org/10.1002/14651858.CD007169.pub2.
Brett, J., Staniszewska, S., Mockford, C., Herron‐Marx, S., Hughes, J., Tysall, C., & Suleman, R. (2014). Mapping the impact of patient and public involvement on health and social care research: A systematic review. Health Expectations, 17(5), 637-650, https://doi.org/10.1111/j.1369-7625.2012.00795.x.
Brotons, M., & Marti, P. (2003). Music therapy with Alzheimer's patients and their family caregivers: A pilot project. Journal of Music Therapy, 40(2), 138-150, https://doi.org/10.1093/jmt/40.2.138.
Canga, B., Hahm, C. L., Lucido, D., Grossbard, M. L., & Loewy, J. V. (2012). Environmental music therapy: A pilot study on the effects of music therapy in a chemotherapy infusion suite. Music and Medicine, 4(4), 221-230, https://doi.org/10.1177/1943862112462037.
Clair, A. A., & Ebberts, A. G. (1997). The effects of music therapy on interactions between family caregivers and their care receivers with late stage dementia. Journal of Music Therapy, 34(3), 148-164, https://doi.org/10.1093/jmt/34.3.148.
Crawford, M. J., Rutter, D., Manley, C., Weaver, T., Bhui, K., Fulop, N., & Tyrer, P. (2002). Systematic review of involving patients in the planning and development of health care. BMJ, 325(7375), 1263, https://doi.org/10.1136/bmj.325.7375.1263.
Cripps, C., Tsiris, G., & Spiro, N. (2016). Outcome measures in music therapy: A free online resource by the Nordoff Robbins Research Team. Nordoff Robbins.
Daykin, N. (2016). Arts for health and wellbeing: An evaluation framework. Public Health England.
DeNora, T. (2006). Evidence and effectiveness in music therapy: Problems, possibilities and performance in health contexts. British Journal of Music Therapy, 20(2), 81-99, https://doi.org/10.1177/135945750602000203.
DeNora, T., & Ansdell, G. (2014). What can’t music do? Psychology of Well-Being: Theory, Research and Practice, 23(4), 1-10, http://www.psywb.com/content/pdf/s13612-13014-10023-13616.pdf.
Geretsegger, M. (2019). Resonating research – What is needed to make music therapy research and implementation more relevant, meaningful, and innovative? Keynote presentation at the 11th European Music Therapy Conference, 26-30 Demark 2019, Aalborg, Denmark. https://www.musictherapy.aau.dk/emtc19/keynotes/#357990.
Gold, C., & Bieleninik, Ł. (2018). Authors’ response. Nordic Journal of Music Therapy, 27(1), 90-92, https://doi.org/10.1080/08098131.2018.1398988.
Graham-Wisener, L., Watts, G., Kirkwood, J., Harrison, C., McEwan, J., Porter, S., Reid, J., & McConnell, T. H. (2018). Music therapy in UK palliative and end-of-life care: a service evaluation. BMJ Supportive & Palliative Care, https://doi.org/10.1136/bmjspcare-2018-001510.
Health and Care Professions Council (HCPC). (2013). The standards of proficiency for arts therapists. https://www.hcpc-uk.org/standards/standards-of-proficiency/arts-therapists/.
Hilliard, R. (2006). The effect of music therapy sessions on compassion fatigue and team building of professional hospice caregivers. Arts in Psychotherapy, 33, 395-401, https://doi.org/10.1016/j.aip.2006.06.002.
Jacobsen, S. L., Waldon, E. G., & Gattino, G. (Eds.). (2019). Music therapy assessment: theory, research, and application. Jessica Kingsley Publishers.
Kaenampornpan, P. (2015). The inclusion of the family members as primary carers in music therapy sessions with children in a special education centre; How does this help the child and the carer? (Doctoral dissertation). Anglia Ruskin University. https://arro.anglia.ac.uk/550334/.
Kent, H., & Read, J. (1998). Measuring consumer participation in mental health services: Are attitudes related to professional orientation? International Journal of Social Psychiatry, 44(4), 295-310, https://doi.org/10.1177/002076409804400406.
Knapp, C., Madden, V., Wang, H., Curtis, C., Sloyer, P., & Shenkman, E. (2009). Music therapy in an integrated pediatric palliative care program. American Journal of Hospice and Palliative Medicine, 26(6), 449-455.
Ledger, A. (2010). Am I a founder or am I a fraud? Music therapists’ experiences of developing services in healthcare organizations. University of Limerick, Ireland. Doctoral dissertation, https://ulir.ul.ie/handle/10344/1131.
Levin-Rozalis, M. (2003). Evaluation and research: Differences and similarities. The Canadian Journal of Program Evaluation, 18(2), 1-31.
Magill, L. (2009). Caregiver empowerment and music therapy: Through the eyes of bereaved caregivers of advanced cancer patients. Journal of Palliative care, 25(1), 68, https://doi.org/10.1177/082585970902500114.
McCaffrey, T. (2018). Evaluating music therapy in adult mental health services: Tuning into service user perspectives. Nordic Journal of Music Therapy, 27(1), 28-43, https://doi.org/10.1080/08098131.2017.1372510.
McLaughlin, D., Barr, O., McIlfatrick, S., & McConkey, R. (2014). Service user perspectives on palliative care education for health and social care professionals supporting people with learning disabilities. BMJ Supportive & Palliative Care, 5(5), 531-537, http://dx.doi.org/10.1136/bmjspcare-2013-000615.
McWhinney, I. R., Bass, M. J., & Donner, A. (1994). Evaluation of a palliative care service: problems and pitfalls. BMJ, 309(6965), 1340-1342, https://doi.org/10.1136/bmj.309.6965.1340.
Michalos, A. C. (2014). Encyclopedia of quality of life and well-being research. Springer.
Minogue, V., Boness, J., Brown, A., & Girdlestone, J. (2005). The impact of service user involvement in research. International Journal of Health Care Quality Assurance, 18(2), 103-112, https://doi.org/10.1108/09526860510588133.
NHS Health Research Authority. (2013). Defining research. https://researchsupport.admin.ox.ac.uk/sites/default/files/researchsupport/documents/media/defining-research.pdf.
O’Callaghan, C., Forrest, L., & Wen, Y. (2015). Music therapy at the end of life. In B. Wheeler (Ed.), Music therapy handbook (pp. 468-480). Guildford Press.
O'Callaghan, C., & Magill, L. (2009). Effect of music therapy on oncologic staff bystanders: A substantive grounded theory. Palliative & Supportive Care, 7(2), 219-228, https://doi.org/10.1017/S1478951509000285.
O'Kelly, J., & Koffman, J. (2007). Multidisciplinary perspectives of music therapy in adult palliative care. Palliative medicine, 21(3), 235-241, https://doi.org/10.1177/0269216307077207.
Omeni, E., Barnes, M., MacDonald, D., Crawford, M., & Rose, D. (2014). Service user involvement: Impact and participation: A survey of service user and staff perspectives. BMC Health Services Research, 14(1), 491, https://doi.org/10.1186/s12913-014-0491-7.
Pavlicevic, M., & Ansdell, G. (Eds.). (2004a). Community music therapy. Jessica Kingsley Publishers.
Pavlicevic, M., & Ansdell, G. (2004b). Introduction: The ripple effect. In M. Pavlicevic & G. Ansdell (Eds.), Community music therapy (pp. 15-31). Jessica Kingsley Publishers.
Pavlicevic, M., O’Neil, N., Powell, H., Jones, O., & Sampathianaki, E. (2014). Making music, making friends: Long-term music therapy with young adults with severe learning disabilities. Journal of Intellectual Disabilities, 18(1), 15-19, https://doi.org/10.1177/1744629513511354.
Pavlicevic, M., Tsiris, G., Wood, S., Powell, H., Graham, J., Sanderson, R., Millman, R., & Gibson, J. (2015). The ‘ripple effect’: Towards researching improvisational music therapy in dementia care homes. Dementia, 14(5), 659-679, https://doi.org/10.1177/1471301213514419.
Powell, H. (2006). The voice of experience: Evaluation of music therapy with older people, including those with dementia, in community locations. British Journal of Music Therapy, 20(2), 109-120, https://doi.org/10.1177/135945750602000205.
Rickson, D. (2009). Researching one’s own clinical practice: Managing multiple roles in an action research project. Voices: A World Forum for Music Therapy, 9(1), https://voices.no/index.php/voices/article/view/364, https://doi.org/10.15845/voices.v9i1.364.
Rolvsjord, R. (2010). Resource-oriented music therapy in mental health care. Barcelona Publishers.
Sargeant, A., Payne, S., Gott, M., Small, N., & Oliviere, D. (2007). User involvement in palliative care: Motivational factors for service users and professionals. Progress in Palliative Care, 15(3), 126-132, https://doi.org/10.1179/096992607X196060.
Solli, H. P., Rolvsjord, R., & Borg, M. (2013). Toward understanding music therapy as a recovery-oriented practice within mental health care: A meta-synthesis of service users' experiences. Journal of Music Therapy, 50(4), 244-273, https://doi.org/10.1093/jmt/50.4.244.
Spiro, N., & Tsiris, G. (2017). Learning from service evaluation: Identifying `impact areas' of music therapy services. In M. Mercadal-Brotons & A. Clements-Cortes (Eds.), Proceedings of the 15th World Congress of Music Therapy; Special Issue of Music Therapy Today (pp. 148-149).
Spiro, N., & Tsiris, G. (2016). Assessment and evaluation in music therapy: Is there a difference? Nordic Journal of Music Therapy, 25(sup1), 70-71, https://doi.org/10.1080/08098131.2016.11783620.
Spiro, N., Tsiris, G., & Cripps, C. (2018). A systematic review of outcome measures in music therapy. Music Therapy Perspectives, 36(1), 67-78, https://doi.org/10.1093/mtp/mix011.
Stige, B., & Aarø, L. E. (2012). Invitation to community music therapy. Routledge.
Stige, B., Ansdell, G., Elefant, C., & Pavlicevic, M. (2010). Where music helps: Community music therapy in action and reflection. Ashgate.
Stige, B., Malterud, K., & Midtgarden, T. (2009). Toward an agenda for evaluation of qualitative research. Qualitative Health Research, 19(10), 1504-1516, https://doi.org/10.1177/1049732309348501.
Storm, M., Knudsen, K., Davidson, L., Hausken, K., & Johannessen, J. O. (2011). “Service user involvement in practice”: The evaluation of an intervention program for service providers and inpatients in Norwegian Community Mental Health Centers. Psychosis, 3(1), 29-40, https://doi.org/10.1080/17522439.2010.501521.
Tsiris, G., Dives, T., & Prince, G. (2014b). Music therapy: Evaluation of staff perceptions at St Christopher’s Hospice. European Journal of Palliative Care, 21(2), 72-75.
Tsiris, G., & Hartley, N. (2014). Research and Evaluation. In N. Hartley (Ed.), End of Life Care: A Guide for Therapists, Artists and Arts Therapists (pp. 227-254). Jessica Kingsley Publishers.
Tsiris, G., & McLachlan, J. (2019). Evaluating music therapy services in children’s hospices. In A. Ludwig (Ed.), Music therapy in children’s palliative care (pp. 67-85). Jessica Kingsley Publishers.
Tsiris, G., Pavlicevic, M., & Farrant, C. (2014a). A guide to evaluation for arts therapists and arts & health practitioners. Jessica Kingsley Publishers.
Tsiris, G., Spiro, N., & Pavlicevic, M. (2018). Repositioning music therapy service evaluation: A case of five Nordoff-Robbins music therapy service evaluations in neuro-rehabilitation. Nordic Journal of Music Therapy, 27(1), 3-27, https://doi.org/10.1080/08098131.2016.1273966.
Turry, A. (2018). Response to effects of improvisational music therapy vs. enhanced standard care on symptom severity among children with autism spectrum disorder: The TIME-A randomized clinical trial. Nordic Journal of Music Therapy, 27(1), 87-89, https://doi.org/10.1080/08098131.2017.1394902.
Wigram, T. (2006). Response to Tia DeNora. British Journal of Music Therapy, 20(2), 93-96, https://doi.org/10.1177/135945750602000203.
Wigram, T., & Gold, C. (2012). The religion of evidence-based practice: Helpful or harmful to health and wellbeing? In R. MacDonald, G. Kreutz, & L. Mitchell (Eds.), Music, health, and wellbeing (pp. 164-182). Oxford University Press.
Wood, S. (2015). The performance of community music therapy evaluation (Doctoral dissertation). Nordoff Robbins/City University London, UK.
Downloads
Additional Files
Pubblicato
Come citare
Fascicolo
Sezione
Licenza
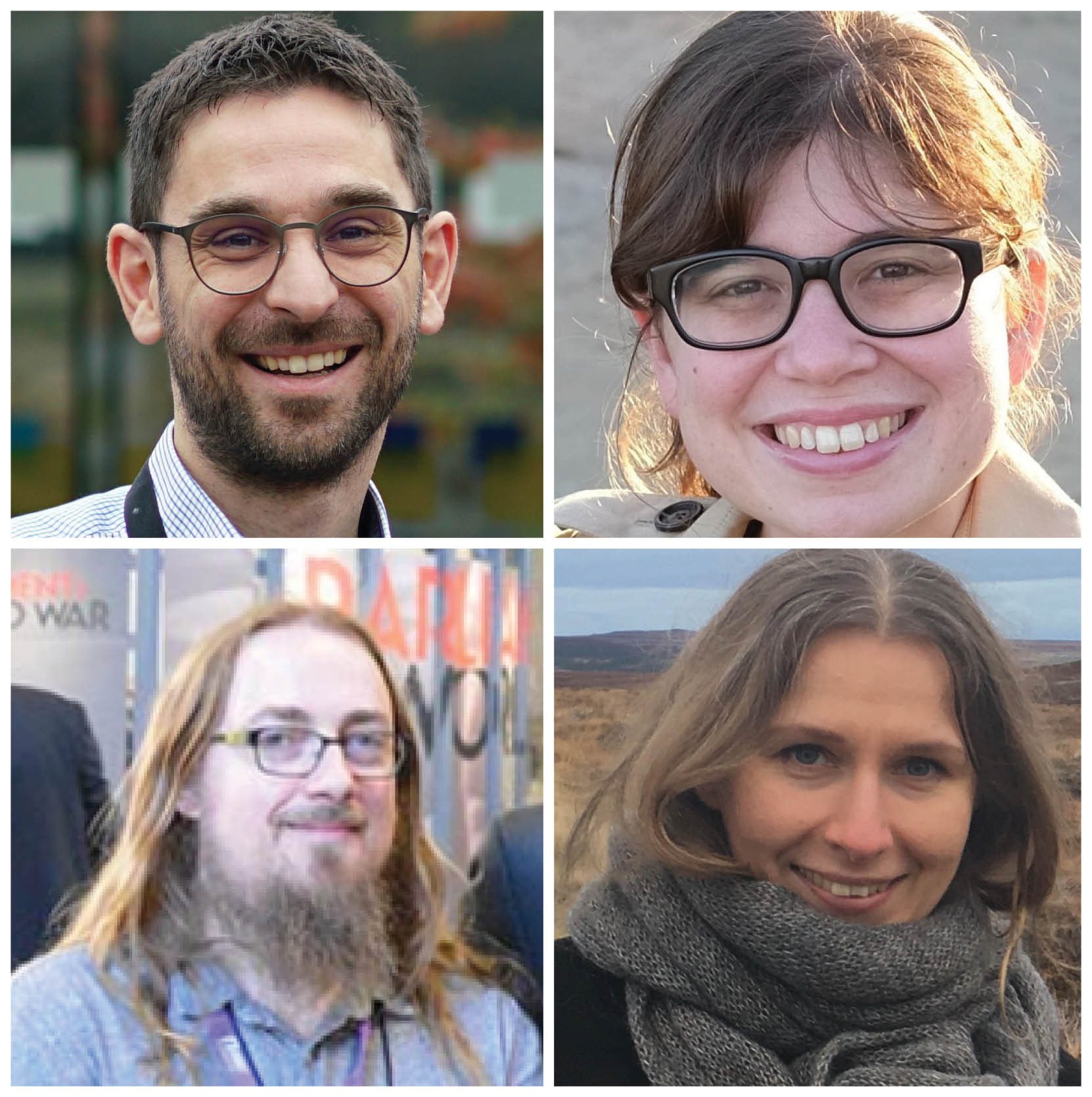
Copyright (c) 2020 Giorgos Tsiris, Neta Spiro, Owen Coggins, Ania Zubala

TQuesto lavoro è fornito con la licenza Creative Commons Attribuzione 4.0 Internazionale.
Articles published prior to 2019 are subject to the following license, see: https://voices.no/index.php/voices/copyright

